Stings Like a Bee
Author: Noopur Basu MD
Peer-Reviewer: Kareem Shahin DO
Final Editor: Katherine Boehm, DO, Will Denq, MD, CAQ-SM
A 16 year old male presents to the ED with complaints of right upper extremity weakness, pain, and paresthesias after falling and striking his head during a football game. No loss of consciousness.
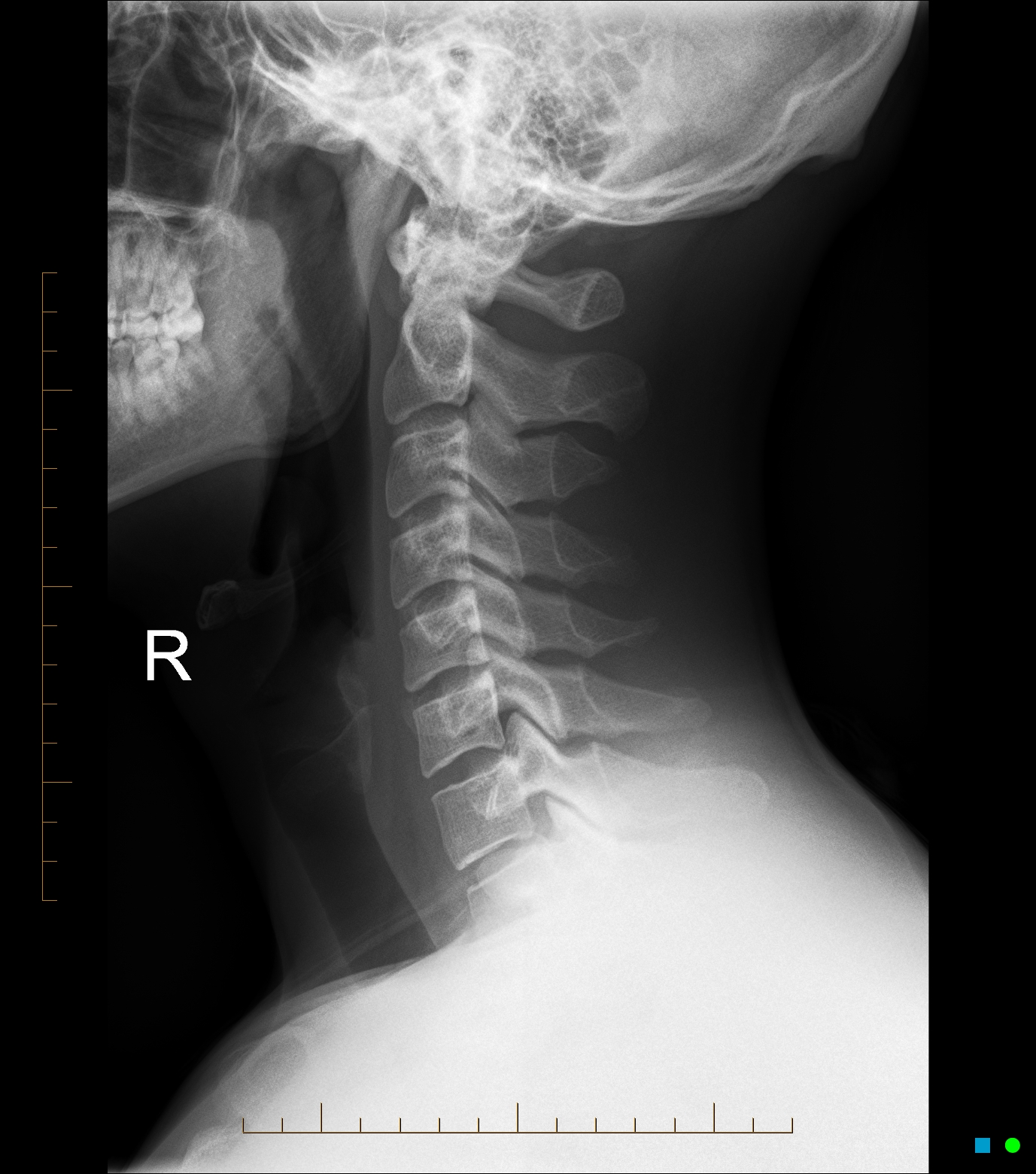
Image 1. Lateral cervical radiograph. Case courtesy of Andrew Dixon, Radiopaedia.org, rID: 32505
What is the diagnosis?
The patient is likely suffering from an acute burner/stinger, also known as “dead arm syndrome”. This is a peripheral nerve injury and a type of brachial plexus injury, typically to the upper trunk.
What is the mechanism of injury?
There are three possible mechanisms of injury: traction injury from stretch, percussive injury from a direct blow, or neck hyperextension with ipsilateral flexion causing direct nerve compression [1-6]. See Image 2 for a brief and traumatizing reminder of the brachial plexus.
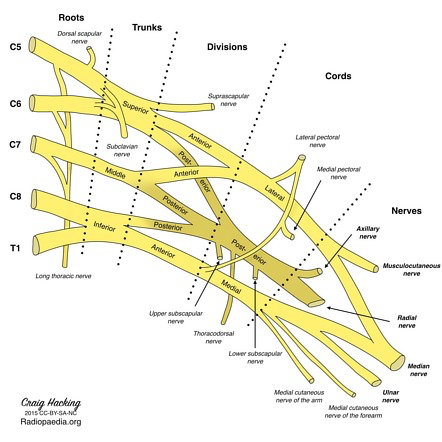
Image 2. Brachial Plexus. Image courtesy of
Craig Hacking , Radiopedia.org rID:37612
What physical exam findings are present?
Transient findings of weakness or sensory abnormalities that can last for up to two days, but often resolve within minutes to hours. Serial examinations may be required. In a true stinger, cervical spine range of motion should be full and intact without midline tenderness. Weakness in the C5 and C6 distribution (deltoid, biceps) can also be present [7].
What imaging modalities can be used?
Utilize clinical decision rules such as the Canadian C-spine or NEXUS criteria to help determine next steps. If the patient still has objective neurologic deficits, computed tomography (CT) should be considered to rule out bony cervical pathology. There is usually no role for emergent MRI for diagnosis [8].
-
Pearl: For a chronic stinger, EMG can be used to assess injury to the roots, cords, trunks, and peripheral nerves if symptoms persist longer than 3 months [7].
What is the management in the ED?
A thorough history and physical examination to evaluate for other serious injuries is pertinent. Rapid resolution of a stinger and lack of prior history of stingers indicates a good prognosis. Reassurance is important as there is no current evidence that there is risk for permanent nerve injury.
When do you consult Orthopedics?
Consultation is not usually warranted unless there are associated bony injuries. In cases of persistent weakness, serial examinations and advanced imaging may warrant consultation or admission - however, this is institutionally dependent.
References
[1] Thein L. Rehabilitation in shoulder injuries. In: Rehabilitation Techniques in Sports Medicine, 2nd ed, Prentice WE (Ed), Mosby-Year Book, Inc, St. Louis 1994. no abstract available
[2] Sallis RE, Jones K, Knopp W. Burners: offensive strategy for an underreported injury Phys Sportsmed. 1992;20:47.
[3] Hershman EB. Injuries to the brachial plexus. In: Athletic Injuries to the Head, Neck, and Face, 2nd ed, Torg JS (Ed), Mosby-Year Book, St. Louis, MO 1991.
[4] Benedetto M, Markey K. Electrodiagnostic localization of traumatic upper trunk brachial plexopathy. D Arch Phys Med Rehabil. 1984;65(1):15.
[5] Markey KL, Di Benedetto M, Curl WW. Upper trunk brachial plexopathy. The stinger syndrome. Am J Sports Med. 1993;21(5):650.
[6] Watkins RG . Neck injuries in football players. Clin Sports Med. 1986;5(2):215.
[7] Schroeder GD, Vaccaro AR. Cervical Spine Injuries in the Athlete. J Am Acad Orthop Surg. 2016 Sep;24(9):e122-33. doi: 10.5435/JAAOS-D-15-00716. PMID: 27479833.
[8] Rihn JA, Anderson DT, Lamb K, Deluca PF, Bata A, Marchetto PA, Neves N, Vaccaro AR. Cervical spine injuries in American football. Sports Med. 2009;39(9):697-708. doi: 10.2165/11315190-000000000-00000. PMID: 19691361.


