You’re Driving Knee Crazy
Author: Madeleine Birch, MD
Peer-Reviewer: Mark Hopkins, MD
Final Editor: Alex Tomesch, MD, CAQ-SM
A 70 year old female presents with knee pain after high speed MVC. Patient felt a “pop” in her knee as it made contact with the dashboard. The “pop” was followed by severe pain and inability to move her right knee. She is tender over her right knee with obvious deformity.


Image 1: Obvious deformity to knee joint upon initial presentation. Image by Mark Hopkins, MD
Image 2: Plain lateral x-ray of right knee [1]
What is the diagnosis?
Posterior Knee dislocation.
What is the mechanism of injury?
High energy trauma is usually required for tibiofemoral dislocation. Dashboard injury in MVC is a common mechanism for posterior knee dislocations [2]. A careful history should be taken because up to 50% of knee dislocations may have been reduced in the pre-hospital setting [3,6].
- Pearl: Four major stabilizers of the knee joint are the anterior and posterior cruciate ligament and the medial and lateral collateral ligaments. A knee dislocation would be expected to disrupt some or all of these ligaments. ACL injury is associated in 75% of cases and the PCL in 95% [8]. Popliteal artery injury occurs in 40% of knee dislocations and peroneal nerve injury in 20% of dislocations [4].
What physical exam findings are expected?
Obvious knee deformities can be immediately present (see Image 1). Gross instability or hyperextension of the joint greater than 30 degrees when the examiner lifts the heel of the affected leg should clue the provider into potential knee dislocation. Type of knee dislocation is classified based on displacement of tibia to femur. [2]
- Pearl: Popliteal, posterior tibial, and dorsalis pedis pulses are key portions of the examination and must be checked if there is concern.
Which imaging modalities can be used?
Emergent evaluation is important as knee dislocations can be limb threatening due to vascular injuries. AP and lateral radiographs are fast and a good initial diagnostic test. ABI is the initial test that should be performed to evaluate for vascular injury. Duplex ultrasonography can be used to evaluate for vascular injuries with a skilled provider or technician, however, CT angiogram is the gold standard diagnostic test of choice. Anybody with decreased ABI, asymmetric pulses, or high suspicion for vascular injury should proceed to CT angiogram. If hard signs of vascular trauma such as absent pulse, cold limb or expanding hematoma are noted, emergent vascular surgery evaluation should be initiated. [3]
- Pearl: Ankle-brachial index (ABI) is beneficial in evaluation. An ABI of 0.9 or greater is considered normal, while an ABI less than 0.9 is suggestive of vascular injury [3]. Concomitant vascular injuries are present in about 3.3% of knee dislocations [7].
What is the difference with artificial joints?
Knee subluxation in artificial joints is uncommon (reported 15 subluxations in more than 3000 primary total knee arthroplasties), but can more easily occur without overt trauma [9]. Posterior subluxations in artificial joints is more common than anterior and is usually associated with ACL and PCL sacrificing surgeries, poor tibial component alignment and pre-existing neurological disorders [9]. As they are less traumatic, they may have fewer concomitant injuries, but keep a high index of suspicion.

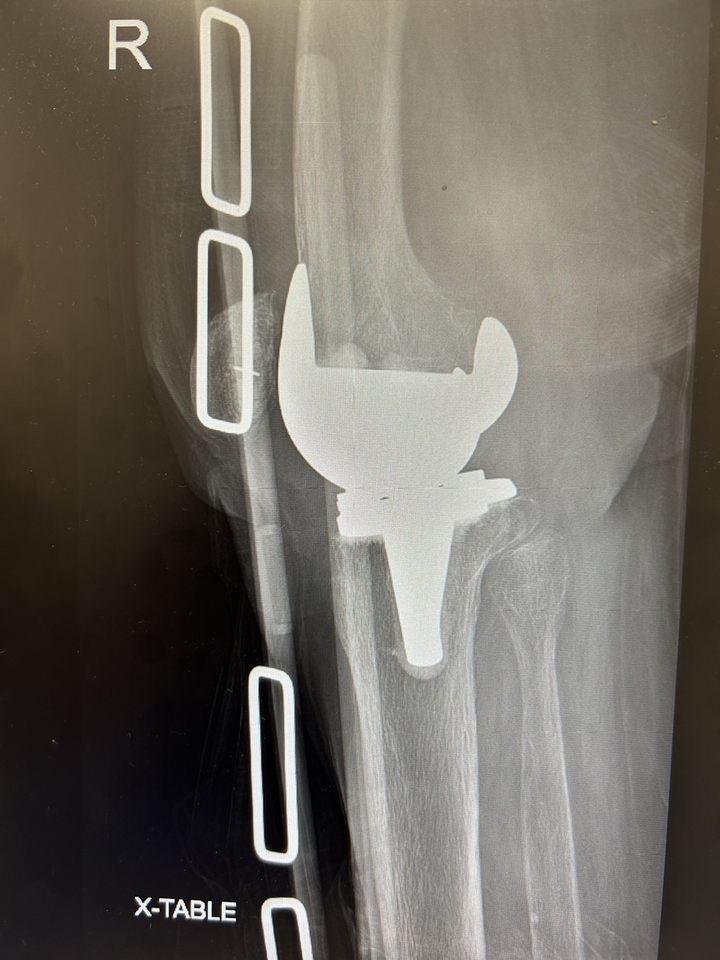
Images 3 and 4, x-ray of posterior subluxation and post-reduction film of prosthetic joint. Courtesy of Mark Hopkins, MD
What is the management in the ED?
Prompt reduction of knee dislocation should be performed in the ED. Appropriate analgesia and sedation should be considered prior to reduction, though reduction should not be delayed, especially if there is concern for a vascular injury. The actual reduction may require multiple people with one person stabilizing the femur while an additional provider manipulates the lower leg. Orthopedics should always be consulted if there is concern for a knee dislocation, as well as potentially vascular surgery if there is popliteal artery injury. If you do not have Orthopedics available to you, likely you will need to transfer the patient for Orthopedic evaluation.
- Pearl: Excessive pressure behind popliteal fossa should be avoided out of caution for causing popliteal arterial injury.
References
[1] Duprey K, Lin M (February 2010). "Posterior knee dislocation". The Western Journal of Emergency Medicine. 11 (1): 103–4. PMC 2850837. PMID 20411095.
[2] Knipe, H., Murphy, A. Knee dislocation. Reference article, Radiopaedia.org. (accessed on 24 Oct 2022) https://doi.org/10.53347/rID-42748 DOI: https://doi.org/10.53347/rID-42748 https://radiopaedia.org/articles/42748 rID: 42748
[3] Fanelli GC. Knee Dislocation and Multiple Ligament Injuries of the Knee. Sports Med Arthrosc Rev. 2018 Dec;26(4):150-152. doi: 10.1097/JSA.0000000000000220. PMID: 30395055.
[4] Karkos CD, Koudounas G, Giagtzidis IT, Mitka MA, Pliatsios I, Papazoglou KO. Traumatic Knee Dislocation and Popliteal Artery Injury: A Case Series. Ann Vasc Surg. 2018 Jul;50:298.e13-298.e16. doi: 10.1016/j.avsg.2018.01.084. Epub 2018 Mar 5. PMID: 29518501.
[5] Mohseni M, Simon LV. Knee Dislocation. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470595/ PMID: 29262122
[6] Gottlieb M, Koyfman A, Long B. Evaluation and Management of Knee Dislocation in the Emergency Department. J Emerg Med. 2019 Nov 8:S0736-4679(19)30826-1. doi: 10.1016/j.jemermed.2019.09.042. Epub ahead of print. PMID: 31711826.
[7] Natsuhara KM, Yeranosian MG, Cohen JR, Wang JC, McAllister DR, Petrigliano FA. What is the frequency of vascular injury after knee dislocation? Clin Orthop Relat Res. 2014 Sep;472(9):2615-20. doi: 10.1007/s11999-014-3566-1. PMID: 24658901; PMCID: PMC4117920.
[8] Kupczik F, Schiavon MEG, Vieira LA, Tenius DP, Fávaro RC. Knee Dislocation: Descriptive Study of Injuries. Rev Bras Ortop. 2013 Jun 20;48(2):145-151. doi: 10.1016/j.rboe.2012.10.002. PMID: 31211120; PMCID: PMC6565857.
[9] Aderinto J, Gross AW, Rittenhouse B. Non-traumatic anterior dislocation of a total knee replacement associated with neurovascular injury. Ann R Coll Surg Engl. 2009 Nov;91(8):658-9. doi: 10.1308/003588409X432509. Epub 2009 Aug 14. PMID: 19686618; PMCID: PMC2966241.


